Antibiotic factories are pumping superbug genes into rivers with no oversight
01/13/2026 / By Cassie B.
- Pharmaceutical factories are discharging wastewater packed with concentrated antibiotic resistance genes directly into the environment.
- This living pollution contains resistance levels up to 100 times higher than normal sewage, creating breeding grounds for superbugs.
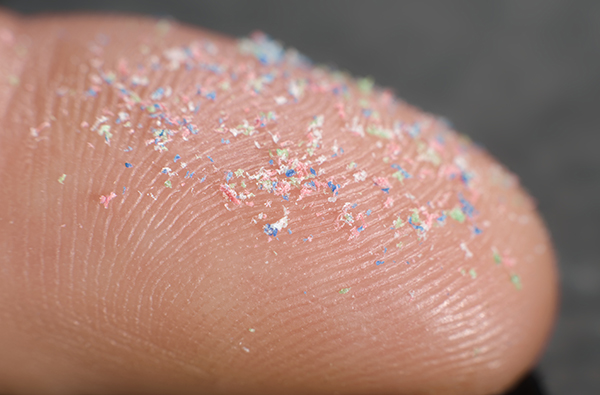
- The genes easily spread between bacteria via mobile genetic elements, acting like biological USB drives.
- This contamination seeps into soils and rivers, entering the food chain and directly threatening human medicine.
- Despite available cleanup technologies, a major regulatory gap means this potent pollution source faces almost no monitoring or mandatory treatment.
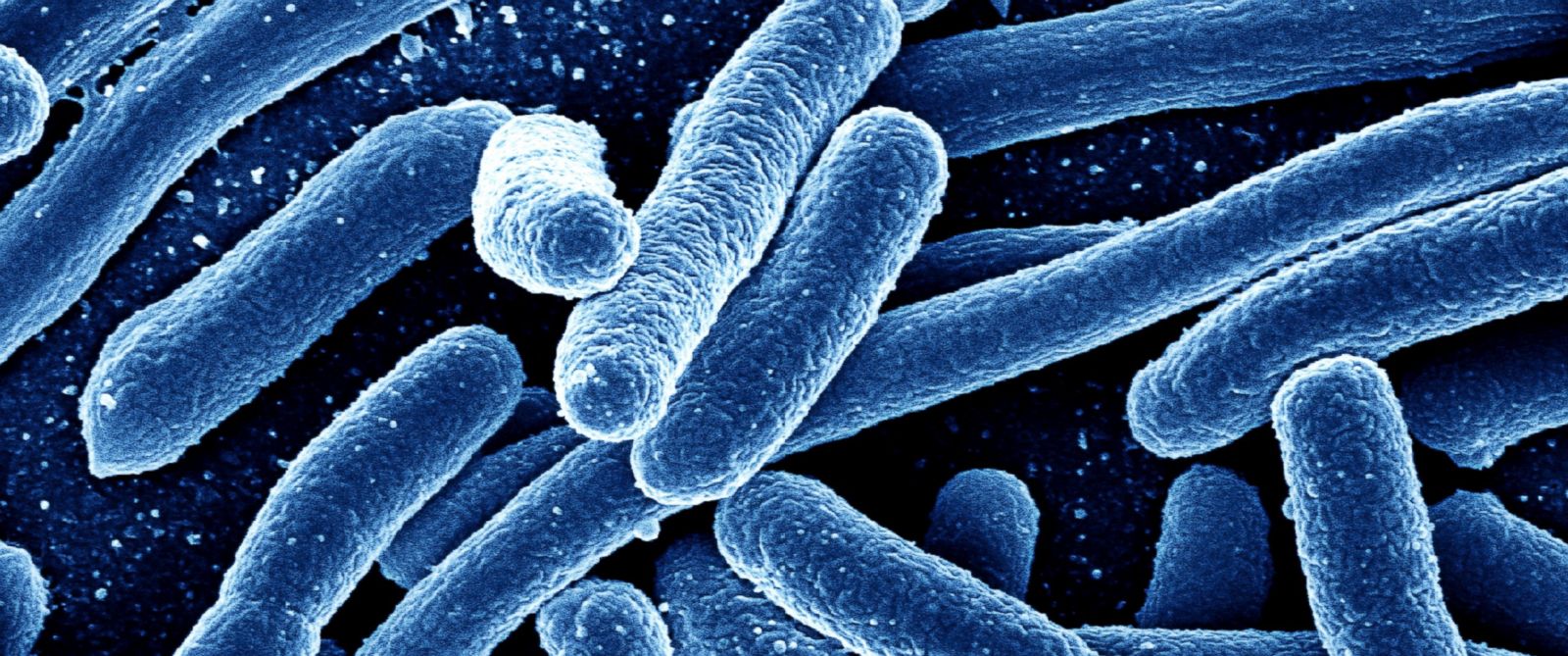
While hospitals and farms face scrutiny for antibiotic overuse, a hidden pollution source is fueling the superbug crisis right at its origin. The factories that manufacture the world’s antibiotics are discharging wastewater packed with concentrated resistance genes directly into the environment, creating ideal breeding grounds for untreatable bacteria.
Research published in the journal Biocontaminant reveals that waste from these pharmaceutical plants contains resistance genes at levels up to 100 times higher than those found in municipal sewage. This isn’t just chemical waste; it’s living pollution. The genes are often attached to mobile genetic elements, which act like biological USB drives, allowing bacteria to easily copy and share instructions for defeating antibiotics.
This industrial effluent flows into rivers and seeps into soils. A study of a sulfonamide drug plant showed downstream soils and river sediments were heavily contaminated, with resistance levels exceeding global averages. This is more than a localized spill; the pollution embeds itself, turning agricultural areas and waterways into reservoirs for resistance.
An evolutionary pressure cooker
The pathway from factory drain to human infection is alarmingly direct. Contaminated rivers water crops. Tainted soil grows food. The resistance genes, once in the environment, can transfer to bacteria that cause common human illnesses. What begins as industrial waste can end up rendering a lifesaving drug useless in a clinic.
What makes this pollution particularly dangerous is its concentrated potency. Antibiotic production creates an extreme evolutionary pressure cooker. Only the toughest bacteria, already armed with multiple resistance tools, survive the process. When these supercharged microbes escape, they can teach their tricks to other bacteria in the environment, including human pathogens.
The regulatory gap is staggering. While global surveillance programs track resistance from hospitals and livestock, pharmaceutical manufacturing faces almost no monitoring for this biological pollution. Current regulations might measure leftover chemical ingredients, but they largely ignore the living, reproducing contamination of resistant bacteria and genes.
The technology exists, but the regulations don’t
Technologies exist to tackle this. Special high-heat composting can eliminate about 90% of antibiotic resistance genes from such waste, while advanced biological treatments can break down antibiotic residues. Yet, no regulations require pharmaceutical companies to deploy these solutions.
This lack of oversight exists despite the known high stakes. Antimicrobial resistance is already linked to an estimated 1.27 million deaths annually. The United Nations Environment Programme has warned that chronically polluted waterways are more likely to harbor microorganisms that foster resistance development.
The problem is a textbook example of a broken system. Pharmaceutical manufacturing operates on a global scale, yet its environmental impact on resistance is a blind spot. A factory in one country can contribute to untreatable infections in another, with no accountability for the pollution it discharges.
The solution requires mandatory, transparent monitoring and treatment standards that address living contamination, not just chemical waste. International cooperation is essential, as the supply chain and the pollution cross all borders.
We are in a race against bacterial evolution, and we are inadvertently arming our opponents at the factory gate. Cleaning up antibiotic production isn’t just an environmental issue; it’s a fundamental requirement for preserving medicine itself for future generations. The technology is ready. The only missing ingredient is the will to regulate.
Sources for this article include:
Submit a correction >>
Tagged Under:
antibiotic resistance, big government, Big Pharma, clean water, Dangerous, Ecology, environ, outrage, pharmaceutical waste, superbugs, suppressed, toxins
This article may contain statements that reflect the opinion of the author
RECENT NEWS & ARTICLES
COPYRIGHT © 2017 ENVIRON NEWS